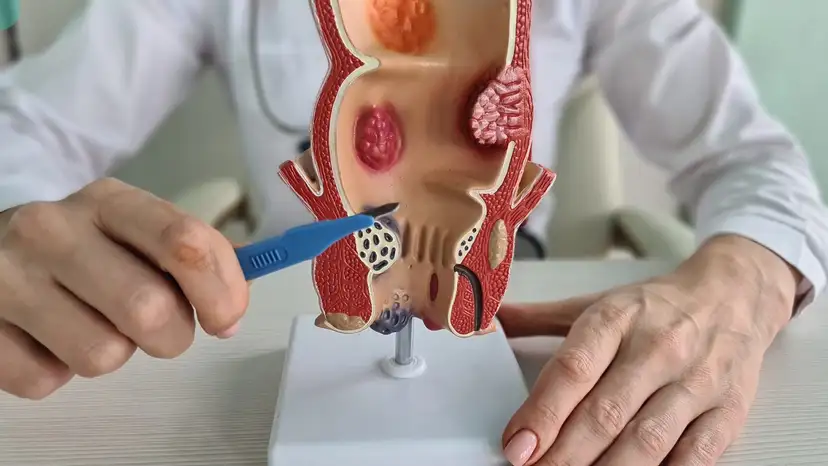
Anal fistulas are small tunnels that form between the end of the bowel and the skin near the anus. They often develop after a previous infection or abscess in the anal glands. These abnormal connections can cause persistent drainage, irritation, and discomfort, making daily activities challenging. Symptoms typically include pain, swelling, redness, discharge of pus or blood, and sometimes a foul odor. Left untreated, anal fistulas can lead to recurrent infections and complications, highlighting the importance of timely medical intervention. Understanding the right surgical approach for your condition can significantly impact recovery, long-term health, and quality of life. This is where the decision between fistulotomy and fistulectomy comes into play.
Anal fistula repair and removal can be achieved through different surgical methods. Doctors often recommend surgery when conservative measures, such as antibiotics or sitz baths, fail to provide relief. Surgical approaches aim to remove the fistula while preserving sphincter function to prevent incontinence. The choice of procedure depends on the fistula’s complexity, location, and patient health. Lifestyle modifications, including proper hygiene, a fiber-rich diet, and avoiding constipation, can complement surgical treatment. Consulting an experienced colorectal surgeon ensures the selection of the most appropriate intervention. Each option has specific benefits, risks, and recovery expectations that patients should fully understand.
Fistulotomy is one of the most commonly performed procedures for anal fistulas. In this procedure, the surgeon carefully opens the fistula tract, allowing it to heal from the inside out. This method is particularly effective for simple, low-lying fistulas that do not involve significant portions of the sphincter muscle. Recovery generally takes a few weeks, during which proper wound care and hygiene are critical to prevent infection. Benefits of fistulotomy include shorter healing time, high success rates, and minimal disruption of normal bowel function. However, there is a small risk of minor incontinence, especially if a larger segment of the sphincter is affected. Patients typically experience mild pain and are advised to maintain a high-fiber diet to avoid straining during bowel movements.
Fistulectomy, on the other hand, involves the complete excision of the fistula tract. This procedure is often recommended for complex or recurrent fistulas that cannot be adequately treated with a simple fistulotomy. Fistulectomy removes the entire infected tissue, reducing the risk of recurrence but often requiring a longer healing period. Postoperative care is crucial, as the larger wound may take more time to close and may require more intensive pain management. Benefits of this procedure include thorough removal of diseased tissue and a lower likelihood of persistent fistula formation. Risks include increased recovery time, potential for temporary incontinence, and higher post-surgical discomfort compared to fistulotomy. Careful patient evaluation and preoperative planning help mitigate these risks.
Comparing fistulotomy and fistulectomy reveals important distinctions.
- Fistulotomy involves opening the tract and letting it heal, while fistulectomy involves complete removal of the tract
- Fistulotomy is typically faster to perform with shorter recovery, whereas fistulectomy may require extended healing
- Simple fistulas are often suitable for fistulotomy, while complex fistulas are more often treated with fistulectomy
- Risk of recurrence is generally higher with fistulotomy for complicated fistulas
- Sphincter function preservation is a major advantage of fistulotomy, but fistulectomy may slightly increase the risk of temporary incontinence
Surgeons consider several factors when choosing the best procedure. Imaging tests, such as MRI or endoanal ultrasound, help determine the fistula’s path and complexity. Fistula location, the amount of sphincter involvement, and the presence of branching tracts influence surgical decision-making. Patient health, including comorbid conditions like diabetes or Crohn’s disease, can also impact recovery outcomes. Shared decision-making between the patient and the colorectal surgeon ensures that individual preferences and lifestyle considerations are included. The goal is to select the surgery that effectively resolves the fistula while minimizing complications. Proper preparation before surgery improves both safety and long-term results.
Preparation for anal fistula surgery plays a significant role in recovery. Patients may be advised to follow a high-fiber diet to prevent constipation and straining during bowel movements. Preoperative hygiene, such as regular sitz baths, helps reduce the risk of infection. Pain management strategies are discussed beforehand to ensure comfort after surgery. Arranging support at home for daily activities is often recommended, especially in the first few days post-surgery. Avoiding smoking and limiting alcohol consumption can further promote healing. Understanding what to expect during recovery reduces anxiety and promotes adherence to post-operative care instructions.
Recovery after surgery varies depending on the procedure and the individual. Wound care involves keeping the area clean, changing dressings as instructed, and monitoring for signs of infection. Pain and discomfort are common but manageable with prescribed medications. Patients are often advised to avoid heavy lifting or strenuous activity for several weeks. Stool softeners or laxatives may be recommended to prevent straining. Regular follow-up appointments allow the surgeon to monitor healing progress and address any complications promptly. Maintaining proper nutrition and hydration supports tissue repair and overall recovery. Emotional support from family or caregivers can also aid in coping with temporary lifestyle adjustments.
Frequently Asked Questions (FAQ)
Which procedure is better for simple anal fistulas?
- Fistulotomy is generally preferred for simple fistulas due to its shorter recovery time and effective healing with minimal risk to sphincter function.
Can fistulotomy or fistulectomy cause incontinence?
- Both procedures carry some risk, but fistulotomy has a lower likelihood. Fistulectomy may temporarily affect continence, particularly for complex fistulas involving more sphincter tissue.
How long does it take to fully recover from each surgery?
- Fistulotomy recovery typically ranges from 4 to 6 weeks, while fistulectomy may require 6 to 8 weeks or longer, depending on the wound size and individual healing rate.
Is one procedure more likely to prevent recurrence?
- Fistulectomy often reduces the risk of recurrence for complex fistulas, while fistulotomy works well for simple cases but may have higher recurrence in complicated scenarios.
Can anal fistulas heal without surgery?
- Minor or superficial fistulas may respond to conservative treatments, but most persistent fistulas require surgical intervention for complete healing.
Are there non-invasive alternatives for fistula repair?
- Some minimally invasive techniques, such as fibrin glue or plug insertion, exist, but their success rates vary and they are not suitable for all fistula types.
Takeaway
Choosing between fistulotomy and fistulectomy requires careful consideration of fistula type, patient health, and personal preferences. Understanding the differences in procedure, recovery, and risks can empower patients to make informed decisions. Consulting an experienced colorectal surgeon ensures the best approach for effective anal fistula repair and removal. Proper preparation, post-operative care, and follow-up monitoring greatly enhance recovery outcomes and reduce the likelihood of recurrence. Whether a simple fistulotomy or a more comprehensive fistulectomy is selected, timely surgical intervention can restore comfort and improve quality of life.